Overview of Angina
Angina is a form of chest pain caused by the decreased blood supply to the heart. A lack of blood flow suggests that the cardiovascular system is not getting enough oxygen. Physical exertion or emotional stress are common causes of this type of discomfort.
The most common symptoms of angina are severe pain and pressure. They might also describe a squeezing feeling in their chest. These senses may last for a few minutes before dissipating. While you climb stairs, exercise, or are stressed, your symptoms may worsen.
With regular exercise or other measures to manage stress, your symptoms may improve. Importantly, in some people, angina can manifest as tiredness, shortness of breath, abdominal discomfort, fatigue, or other symptoms in addition to the "typical" chest discomfort.
Symptoms that show up along with angina
- Pain in the abdomen
- Sweating excessively
- Stomach ache or gas (indigestion)
- Fatigue
- Vomiting and nausea
- Neck, jaw, shoulder, or back pain
- Breathing difficulty (dyspnea)
Angina is more common in men over 45 and women over 55
Secure your health with a second opinion. Make informed decisions and book your appointment today!
Get A Second Opinion
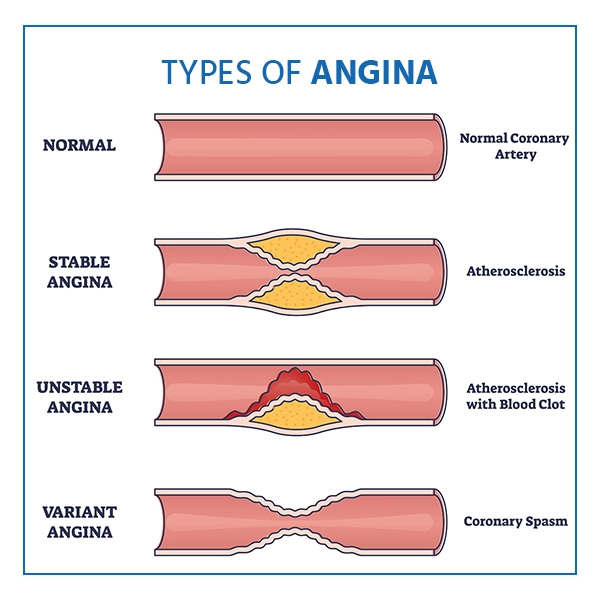
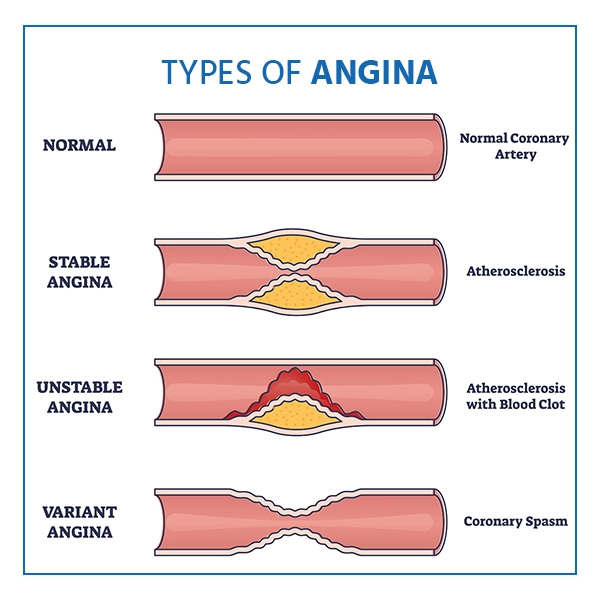
Types of Angina
- Stable Angina: The most frequent type of angina is stable angina, often known as angina pectoris. Stable angina is a well-defined pattern of chest discomfort. The pattern is frequently traceable based on what you're doing while you feel the discomfort in your chest. Tracking stable angina symptoms can help you manage them more readily.
- Unstable Angina: Another type of angina is unstable angina. It happens unexpectedly and worsens with time. It has the potential to result in a heart attack.Although stable angina is less severe than unstable angina, it can still be painful and uncomfortable. Both types of angina are typical symptoms of an underlying heart issue, so consult your doctor as soon as you notice any symptoms.
- Microvascular angina: It can arise in the presence of coronary microvascular dysfunction (MVD). This has an impact on the tiniest coronary arteries, In addition to chest pain, an individual may feel:
- weariness and a lack of energy :
- Sleeping issues
- Breathing difficulty
- Microvascular angina is more likely to be persistent than stable angina. It frequently lasts more than 10 minutes and, on occasion, more than 30 minutes.
- Variant Angina: Variant angina is uncommon. Doctors frequently refer to it as Prinzmetal angina, and it can occur when the body is at rest, usually around midnight or early in the morning.It occurs when the coronary arteries contract. Cold exposure, stress, medications, smoking, or cocaine usage are all potential factors.It is a serious illness that can be treated medically.
Angina symptoms
The symptom is chest pain, but it differs from person to person. One can experience:
- weariness and a lack of energy
- Burning
- Discomfort
- Dizziness
- Fatigue
- A sense of wholeness in your chest
- A sense of tiredness or pressure
- Vomiting or upset stomach
- Breathing difficulty
- Squeezing
- Sweating
You could misunderstand aching or blistering heartburn or gas.
Pain behind your breastbone is likely, and it may spread to one's shoulders, arms, neck, throat, jaw, or back. Rest often helps with stable angina. Unstable angina may not, and it may worsen. It's a medical issue that needs immediate attention.
When to see a doctor?
If your chest pain lasts more than a few minutes and does not go aside when you relax or take your angina medicines, it could be an indication of a heart attack. Call emergency medical assistance. Only start driving yourself to the health center if you have no other option.
If chest uneasiness is a new side effect for you, it's critical to see your doctor to determine the cause and receive proper treatment. If you've been detected with stable angina and it worsens or changes, seek medical attention right away.
Causes
Angina is usually caused by heart disease. Plaque, a fatty substance, accumulates in the arteries, obstructing blood supply to the heart muscle. As a result, your heart must work with much less oxygen. This causes discomfort. You may have blood clots in your heart's arteries, which can lead to heart attacks
The following are some less common causes of chest pain:
- A clog in a major artery leads to the respiratory system (pulmonary embolism)
- A heart that is enlarged or thickened (hypertrophic cardiomyopathy)
- A valve in the main chamber of your heart narrows (aortic stenosis)
- When the sac all over the heart is swollen (pericarditis)
- Tears in the wall of the aorta, the body's largest artery (aortic dissection)
During times of low oxygen demand, such as when resting, the heart muscle may be able to work with less blood circulation without provoking angina symptoms. Angina can occur whenever the demand for oxygen increases, such as when exercising.
Risk factors
The following factors may raise your risk of angina:
- Getting older: Angina is most common in adults over the age of 60.
- Heart disease runs in the family Inform your doctor if your mother, father, or any siblings have or have had cardiovascular disease or a heart attack.
- Tobacco consumption: Smoking, chewing tobacco, and long-term secondhand smoke exposure can harm the lining of the arteries, allowing cholesterol deposits to accumulate and block blood flow.
- Diabetes: Diabetes raises the risk of heart attack, which causes angina and heart attacks by hastening atherosclerosis and elevating cholesterol levels.
- Blood pressure is high: Hypertension damages arteries over time by hastening artery hardening.
- High levels of cholesterol or triglycerides: Too much bad cholesterol, known as low-density lipoprotein (LDL), in the bloodstream can cause artery narrowing. High LDL cholesterol raises the risk of angina and heart disease. A high triglyceride level in the blood is also harmful.
- Other medical conditions: Angina is more likely in people who have chronic kidney problems, peripheral arterial disease, metabolic syndrome, or a history of stroke.
- There isn't enough exercise: Inactivity is linked to high cholesterol, hypertension, type 2 diabetes, and obesity. Consult your doctor about the type and number of exercises that are best for you.
- Obesity: Obesity increases the risk of heart disease, which might lead to angina. Obesity causes the heart to beat to supply blood throughout the body.
Diagnosis
To diagnose angina, your doctor will perform a physical exam and ask you about your health history. You'll also be asked about every risk factor, such as a family history of heart disease.
The following tests are used to identify and confirm angina:
- ECG or EKG stands for electrocardiogram: This simple and painless test assesses the heart's electrical activity.
- X-ray of the chest: A chest X-ray reveals the health of the heart as well as lungs
- Blood tests are performed: These substances can be detected using a cardiovascular enzyme blood test.
- The stress test: A typical stress test consists of walking on a treadmill or trying to ride a stationary bike while the heart rate is monitored.
Treatment
Your treatment will be determined by the extent of the damage to your heart. Medicine and changes in lifestyle can often help people with mild angina, improve their blood flow and control the symptoms.
- Medicines :Your doctor may prescribe the following medications:
- Nitrates and calcium channel blockers relax and widen capillaries, allowing more blood to flow to the heart.
- Beta-blockers slow down your heart, enabling it to work less hard.
- Antiplatelet or blood thinner medications are used to prevent heart attacks and strokes.
- Statins are medications that are used to lower cholesterol and stabilize plaque.
- Therapies: To increase the blood flow to the heart, a non-drug option known as enhanced external counterpulsation (EECP) may be suggested at times. Blood pressure cuffs are wrapped around the calves, thighs, and pelvis during EECP. Multiple treatment sessions are required for EECP. People who have frequent, uncontrolled angina may benefit from EECP (refractory angina)
- Blood tests are performed: These substances can be detected using a cardiovascular enzyme blood test.
- Cardiovascular procedures: If medications are ineffective, you may require a medical procedure or surgery to open blocked arteries. It could be:
- Angioplasty combined with stenting: A small balloon is implanted into the narrowed artery during angioplasty, also known as a percutaneous coronary intervention (PCI). After inflating the balloon to widen the artery, a small wire mesh coil (stent) is typically integrated to keep the artery open.
- Coronary artery bypass procedure (coronary artery bypass surgery): A vein or artery from another part of the body is being used to bypass a blocked artery heart artery during coronary artery bypass surgery.
Do’s and Don’ts of Angina
The symptoms of this disease can be pain in the chest, heart palpitations, and more. Here are some dos and don’ts in this condition that can help you ease the symptoms.
| Do’s |
Don’ts |
| Allow the individual to rest and try to relax |
Delay in seeking medical attention |
| Help the person in seeking medical care |
Make the individual walk or sit |
| Remove any restrictive clothing |
Leave the person experiencing chest pain alone |
| Enquire if the person is taking any prescription medication for a known cardiovascular disease |
Wait for the symptoms to subside |
| Assist the individual in taking the medication |
Give the person anything orally unless it is nitroglycerin/aspirin suggested by any expert |
Follow the dos and don’ts of the Angina disease as it can worsen over time if ignored and may also lead to heart attack or severe cardiovascular disease.
Ready to take control of your health journey? Book your appointment now and start your path towards wellness today!
Book an Appointment
Angina Care at Medicover
At Medicover hospitals, we have the most reliable healthcare team of Cardiologists, Interventional cardiologists, and Electrophysiologists who design a personalized treatment pathway for each patient. We adopt a multi-faceted approach for managing Angina disease with the active participation of healthcare specialists from different departments to address the disease for holistic recovery and wellness. We aim to provide the best treatment outcomes and satisfactory patient experiences at a highly affordable cost.